
What is Hydrocephalus?
The following excerpt is taken from Chapter One of Hydrocephalus: A Guide for Patients, Families, and Friends by Chuck Toporek & Kellie Robinson, copyright 1999 by O'Reilly & Associates, Inc. For book orders/information, call 1-800-998-9938. Permission is granted to print and distribute this excerpt for noncommercial use as long as the above source is included. The information in this article is meant to educate and should not be used as an alternative for professional medical care.
* Introduction
* Types of hydrocephalus
* Primary causes of hydrocephalus
* What is cerebrospinal fluid?
* The brain in a nutshell
Introduction
The word hydrocephalus is derived from the Greek–hydro means water, and cephalus means head. It is a neurological condition that occurs when there is an abnormal accumulation of cerebrospinal fluid (CSF) within the ventricles and/or subarachnoid space of the brain. The increase of intracranial pressure (ICP) can either be the result of an overproduction of CSF (a condition known as choroid plexus papilloma), an obstruction of the flow of CSF, or a failure of the structures of the brain to reabsorb the fluid. Although there is little public awareness about hydrocephalus, according to recent statistics from the U.S. Centers for Disease Control and Prevention, hydrocephalus affects approximately 1 out of every 1,000 children born each year. Hydrocephalus can also be acquired after birth from a variety of causes.
Types of hydrocephalus
Hydrocephalus is a condition where the normal drainage of CSF in the brain is blocked in some way. Neurosurgeons classify hydrocephalus according to when the condition was developed (congenital or acquired), and whether it was caused by a reabsorption problem or a blockage somewhere within the ventricles (communicating or non-communicating). Another type of hydrocephalus–normal pressure hydrocephalus–is when the ventricles are enlarged, but there is little or no increase in intracranial pressure. These terms are often combined when referring to a particular type of hydrocephalus. For example, if you have a condition known as aqueductal stenosis (a blockage of the aqueduct of Sylvius) caused by an intraventricular cyst, then your diagnosis would be "acquired, non-communicating hydrocephalus."
Congenital hydrocephalus
Hydrocephalus is considered congenital when its origin can be traced to a birth defect or brain malformation that causes an increased resistance to the drainage of CSF. A variety of factors can cause congenital hydrocephalus. Among the possible causes:
* Toxoplasmosis, or T gondii, is a type of organism that can be transmitted by eating undercooked meat, contact with contaminated soil, or by direct contact with an animal or bird that already has the infection.
* Cytomegalovirus (CMV) belongs to the herpes family of viruses, and normally produces symptoms that resemble that of the common cold.
* Rubella, or German measles, is known to cause fetal malformations during pregnancy, one of which is hydrocephalus.
* X-linked hydrocephalus is almost exclusively a genetic disorder passed from mother to son on the X chromosome. It is inherited only through the mother, and is predominantly seen in males (approximately one in 20). There is also a small chance that first cousins of children with uncomplicated congenital hydrocephalus can also inherit the disorder.
Congenital hydrocephalus can be linked to other complications. A 17-year study that concluded in 1987 tracked four major congenital neurological malformations: anencephaly, spina bifida, encephaloceles and hydrocephalus. Of 370 births with these defects, 10.5 percent (39) resulted in stillbirths. Although a majority of live-born infants with hydrocephalus were free of other complications, 37 percent had congenital malformations which were unrelated to the hydrocephalus. Of those, the most common malformations were tracheoesophageal fistula (an abnormal communication between the trachea, or windpipe, and the esophagus), and anomalies with the reproductive, urinary, and cardiac systems (Thomas E. Wiswell et al., "Major congenital neurologic malformations: a 17-year study," American Journal of Diseases in Children 144, no. 1, January 1990: 61-7).
Acquired hydrocephalus
Hydrocephalus can be acquired later in life if something causes an increase in the resistance to the drainage of CSF, such as an obstruction. Acquired hydrocephalus can also be caused by brain tumor, arachnoid cyst, intracranial or intraventricular hemorrhaging (IVH), trauma to the head, or by infections such as meningitis.
At the age of six weeks, my mom noticed that my head was unusually large, and she could lay a finger between the bones in my skull. She called the neurosurgeon, and met him in the emergency room. He saw me from across the examination room, proceeded to the phone, and reserved time in the operating room. To him, it was very apparent that I was in dire need of a shunt. My head was about the size of the rest of my body.
In 1983, at the age of thirteen, I acquired hydrocephalus when I was hit in the head by a baseball. It was a freak accident. I was a good player, and could hit and field well. Unfortunately, that one time the ball was thrown to me, I looked up and lost it in the sun. My nose bled and immediately swelled; my family and I just assumed that I broke my nose again. Only later did we realize the true complications that occurred.
I went to the doctor and he confirmed that my nose was broken. However, there was nothing he could do at that time. It would have to just heal on its own. Approximately a month later, I missed school because I was very lethargic and had excruciating headaches. At first, they thought that it might be migraine headaches, however, as I grew more lethargic and bright lights started to bother me, my family grew very concerned.
Since it was at the end of my freshman year in high school, I did not want to miss much school, so I tried to “work” through the illness. However, when the nausea increased and my vision doubled, I went to my pediatrician, who sent me to the hospital for tests and a CT scan. As the result of my scans, I was sent to the Children's Hospital in Boston. It was there that I was diagnosed with hydrocephalus.
Bacterial meningitis
Bacterial meningitis is an inflammation of the meninges, the protective layering that surrounds the brain and spinal cord. Hydrocephalus develops when scarring of the meninges restricts the flow of CSF in the subarachnoid space, when it passes through the aqueduct of the ventricular system, or affects the absorption of CSF at the arachnoid villi.
If left untreated, bacterial meningitis can cause death within days. Signs and symptoms of meningitis include: severe headaches, high fever, loss of appetite, light and sound sensitivity, and tension in the muscles of the neck and shoulders. In extreme cases, symptoms of meningitis can include vomiting, convulsions or seizures, and delirium. Once detected, bacterial meningitis can be treated with high doses of antibiotics.
Brain tumors and cysts
Hydrocephalus may also be acquired as a result of brain tumors or cysts. Most brain tumors are detected in children between the ages of five and ten years old. Seventy-five percent of these tumors occur in an area at the back of the brain, known as the posterior fossa. Other types of brain tumors that can cause hydrocephalus include intraventricular tumors, and in extremely rare cases, tumors of the choroid plexus (including papilloma and carcinoma).
As the tumor grows in mass, it creates a form of non-communicating hydrocephalus by reducing the flow of CSF within the ventricles. Tumors that are located in the back of the brain most commonly obstruct the flow of CSF through and out of the fourth ventricle. In most cases, the best way to treat hydrocephalus related to a tumor is to remove (excise) the tumor causing the obstruction. However, hydrocephalus does persist in approximately 20 to 40 percent of patients after the tumor is removed.
Cysts are benign sacs or closed cavities that are filled with fluid. Cysts can occur anywhere in the body. With arachnoid cysts, the sacs are filled with CSF and are lined with tissue from the arachnoid membrane. Cysts are commonly found in children, and are located both within the ventricles and on the surface of the brain, or in the subarachnoid spaces. Arachnoid cysts can cause a form of non-communicating hydrocephalus by restricting the flow of CSF within the ventricular system–particularly in the third ventricle. Cysts can also be found in the subarachnoid space.
Depending on the location of the cyst, the neurosurgeon may be able to excise the cyst wall and drain the cyst's fluid. If the cyst is located in an inoperable location (e.g., near the brain stem), the neurosurgeon might decide to place a shunt catheter in the cyst. This catheter is then connected to a shunt system to allow the fluid to be drained. This stops the growth of the cyst and protects the brain stem.
Intraventricular hemorrhages (IVH)
A common complication with premature births is the risk of an intracranial or intraventricular hemorrhage (IVH), bleeding within the ventricles of the brain. IVHs can be found in approximately 40 percent of premature infants. If the IVH is severe enough, it could compromise the ventricles, allowing blood to flow into surrounding brain tissues and lead to neurological changes. The possibility of hydrocephalus developing as a result of an IVH depends largely on the severity of the bleed, and whether or not blood and debris have caused an obstruction in the CSF pathways, or reduced the brain's ability to reabsorb the CSF. In many cases, however, hydrocephalus is mild and tends to stabilize. Thus, not all infants who have an IVH will need a shunt system.
Head trauma
Severe head trauma can also cause hydrocephalus, although it is uncommon. The hydrocephalic condition occurs as a result of bleeding into the subarachnoid spaces. Scarring of the drainage pathways from the resulting intracranial bleed can cause a partial obstruction of the flow of CSF.
Communicating hydrocephalus
The term "communicating hydrocephalus" means that the site of increased resistance to CSF drainage resides outside of the ventricular system in the subarachnoid space. Communicating hydrocephalus is caused one of three ways:
* An overproduction of CSF (a rare condition associated with a choroid plexus papilloma).
* A venous obstruction (a rare condition known as Otitic hydrocephalus).
* An increased resistance to the drainage of CSF from the subarachnoid space.
"Communicating" means the ventricles of the brain communicate, or pass along, the CSF to the surface of the brain. The obstruction of CSF flow occurs not within the ventricles, but within the subarachnoid spaces of the brain. Communicating hydrocephalus can also be the result of a meningeal inflammation, such as an infection, or by blood or tumor cells in the subarachnoid spaces.
Non-communicating hydrocephalus
Non-communicating, or obstructive, hydrocephalus is caused when there is an obstruction in the flow of CSF within the ventricular system of the brain, including the outlets of the fourth ventricle (the foramina of Luschke and Magendie). The most common place for the non- communicating CSF obstruction is in the aqueduct of Sylvius (also known as aqueductal stenosis). However, the obstruction can also occur in the outlets of the fourth ventricle and from the lateral ventricles into the third ventricle at the foramina of Monro.
An example of non-communicating hydrocephalus is stenosis (or blockage) of the aqueduct of Sylvius. This blockage causes non-communicating hydrocephalus by not permitting CSF to flow from the third to the fourth ventricle. When the obstruction is located in the ventricular system, it causes the ventricles to expand as a result of the accumulation of CSF. Non-communicating hydrocephalus is the most common form of hydrocephalus in fetuses.
Normal-pressure hydrocephalus (NPH)
A person can be diagnosed as having normal pressure hydrocephalus (NPH) when the ventricles of the brain are enlarged, but there is little or no increase in the pressure within the ventricles. NPH is normally seen in elderly patients, and is most likely caused by an obstruction of the CSF pathways and abnormal brain compliance.
NPH can be divided into two classifications: those where the cause of the hydrocephalus is known, such as a previous history of meningitis or a subarachnoid hemorrhage, and idiopathic, where the cause of NPH is not known.
Management of NPH can often be tricky, as the neurosurgeon must try to find the right shunt to treat the condition. If the shunt overdrains, it could result in a subdural accumulation, or pocket, of CSF and/or blood between the dura and arachnoid mater of the meninges. If the shunt doesn't drain enough CSF (known as undershunting), the ventricles may not be allowed to reduce in size. Also, shunting may not improve the situation.
Primary causes of hydrocephalus
Although hydrocephalus can develop for a variety of reasons, congenital hydrocephalus is often a part of other neurological conditions and congenital malformations. Other conditions that hydrocephalus is often associated with include, from most to least common:
* Dandy-Walker syndrome.
* Neural tube defects (NTDs).
* Spina bifida.
* Chiari malformations.
* Vein of Galen malformations.
* Hydranencephaly.
* Craniosynostosis.
* Schizencephaly.
This section briefly describes these disorders and explains how they can cause hydrocephalus, as well as symptoms, treatments and prognosis. For more detailed information, talk with your doctor or neurosurgeon, as she can provide more detailed information as it pertains to your child.
Dandy-Walker syndrome
Dandy-Walker syndrome is a congenital brain malformation that involves the fourth ventricle and the cerebellum. It is defined as an enlargement of the fourth ventricle, and is accompanied by an absence (partial or complete) of the cerebellar vermis (the narrow middle area between the hemispheres of the brain). The combination of these malformations is what causes hydrocephalus in patients with Dandy-Walker syndrome.
Symptoms that often occur in early infancy include slow motor development and progressive macrocephaly (an abnormally enlarged skull). In older children, symptoms of increased intracranial pressure such as irritability, vomiting, and/or signs of cerebellar dysfunction such as ataxia (unsteady gait) and nystagmus (jerky eyes) may occur.
Symptoms of Dandy-Walker syndrome include increased head circumference, bulging occiput (the back of the head), cranial nerve dysfunction, and abnormal breathing patterns. Dandy-Walker syndrome can be associated with other central nervous system structural abnormalities, including malformations of the heart and an absence of the corpus callosum.
In cases where increased intracranial pressure is present, a shunt will most likely be placed to control the hydrocephalus. Even when hydrocephalus is treated early, patients with Dandy-Walker syndrome often face other problems. Prognosis for normal intellectual development is variable depending on the severity of the syndrome and its associated malformations.
Neural tube defects
Spina bifida (SB) is a general term that denotes failure of normal formation of midline structures–in this case, the spinal cord and the spinal column. Those conditions that are of clinical importance include only the neural tube and are collectively referred to as neural tube defects (NTDs). NTDs are best divided into two groups: open and closed.
* Open NTDs. These are found in infants with myelomeningoceles. The spinal cord is open and is continuously or intermittently leaking CSF. The entire CNS is malformed, and the myelomeningoceles is likened to the tip of the iceberg above the waterline.
These infants have a partial or complete paralysis of the lower extremities, which may also be deformed. Bladder and bowel function are almost always severely affected with the infant never becoming continent for urine or stool. The vast majority of infants develop progressive hydrocephalus and will need to be shunted. Because of cortical disorganization, the majority of children will have learning disorders that vary from mild to severe. The medical care required is complex and lifelong.
* Closed NTDs. The spinal cord is not exposed, but is covered by skin. CSF leakage is not present. The abnormality is confined to the lower end of the spinal cord, and there is no malformation of the brain. Thus, the Chiari malformation, hydrocephalus, and learning disorders are not a consideration. These infants can develop bladder and/or bowel dysfunction and a mild motor/sensory loss that normally involves only one lower extremity.
At present, there is no cure for myelomeningoceles because the nerve tissue cannot be replaced or repaired. Surgery to close the newborn's spinal opening is generally performed within two days of birth to minimize the risk of infection and to preserve existing function in the spinal cord. Ongoing therapy, medical care, and surgical treatments may be necessary to prevent and manage complications throughout the person's life. Many individuals with myelomeningoceles will need assisting devices such as braces, crutches, or wheelchairs.
The prognosis for children with myelomeningoceles depends on the number and severity of other abnormalities. Prognosis is poorer for those with complete paralysis, hydrocephalus, and other congenital defects. With proper medical care, most children with myelomeningoceles live well into adulthood.
Chiari malformation (CM)
A Chiari malformation (CM; formerly referred to as Arnold-Chiari malformation, or ACM) is a rare congenital anomaly in which two parts of the brain–the brain stem and the cerebellum–are longer than normal and protrude down into the spinal canal. Chiari malformations are divided into two groups:
* Type I. A mild form with the cerebellar tonsils protruding into the spinal cord. This may be asymptomatic or be associated with cranial nerve dysfunction or fluid build-up in the spinal cord (hydrosyringomyelia).
* Type II. A more severe form with an extensive malformation of the cerebellum and brain stem that is seen almost exclusively with an open NTD (i.e., myelomeningoceles). Hydrocephalus is usually present. Some infants may develop difficulty with breathing, swallowing, feeding, etc., as a result of this malformation.
Most patients who have surgery experience an improvement of symptoms almost immediately, and may experience prolonged periods of relative stability, while others may continue to have neurological deterioration. Infants with severe malformations may have life-threatening complications.
Vein of Galen malformation (VGM)
The vein of Galen malformation (VGM) is a rare vascular disorder that is present at birth, but normally isn't detected until the child is a few months old. VGMs occur when the vein of Galen, which runs above the aqueduct of Sylvius, balloons to create an aneurysimal sac. This aneurysm often compresses the aqueduct of Sylvius, causing hydrocephalus.
Vein of Galen malformations are commonly diagnosed in infants by a cardiologist, as the infant often suffers heart failure (a heart attack) because of the rapid rate of heart circulation. Another symptom that aids in the detection and diagnosis of a VGM is macrocrania (an enlarged skull). Macrocrania is caused when the ventricles enlarge due to the obstruction of CSF flow, causing increased intracranial pressure.
Symptoms often include headache (due to increased intracranial pressure), lethargy (due to an enlarged heart), and vomiting. One of the primary concerns in the diagnosis of a VGM is the enlarged heart, which may lead to heart failure. VGMs are easily diagnosed with contrast- enhanced CT or MRI. X-rays of the chest will confirm whether the heart is enlarged or not.
Shunting is often required to treat the hydrocephalus, but may not be necessary if ICP is reduced when the VGM is treated.
Hydranencephaly
Hydranencephaly is a rare condition in which the brain's cerebral hemispheres are absent and are replaced by sacs filled with cerebrospinal fluid. An infant with hydranencephaly may appear normal at birth. The infant's head size and spontaneous reflexes, such as sucking, swallowing, crying, and moving the arms and legs may all be normal.
Due to the lack of cerebral hemispheres, there is no significant neurological development, with the infant's function remaining at the newborn level forever. Hydrocephalus frequently develops, and a shunt is inserted to keep the child's head from becoming abnormally large.
Diagnosis may be delayed for several months because early behavior appears to be relatively normal. Some infants may have additional abnormalities at birth, including seizures, myoclonus (spasm or twitching of a muscle or group of muscles), and respiratory problems. There is no definitive treatment for hydranencephaly other than to place a shunt to prevent the head from becoming large, and surgery to treat other malformations.
Craniosynostosis
Craniosynostosis is a congenital anomaly which is characterized by the premature closure of one or more cranial sutures before the brain has fully grown. The disorder results in an abnormal head shape, and may be a feature of a chromosomal or genetic syndrome or abnormality. Treatment for craniosynostosis generally consists of surgery, usually performed early in life. This allows the skull to accommodate brain growth, and improves the appearance of the child's head.
Prognosis for craniosynostosis varies depending on whether single or multiple sutures are involved and the presence of associated abnormalities. The prognosis is generally better for patients with single suture involvement and no associated abnormalities. Hydrocephalus is rarely present with single-suture involvement, and is occasionally seen with some other forms of craniosynostosis.
Schizencephaly
Schizencephaly is an extremely rare developmental disorder characterized by abnormal slits, or clefts, in the brain's cerebral hemispheres. Individuals with clefts in both hemispheres (bilateral clefts) are commonly developmentally delayed, and have delayed speech and language skills. Individuals with smaller, unilateral clefts (clefts in only one hemisphere) are often paralyzed on one side of the body and may have normal intelligence. Patients with schizencephaly may also have varying degrees of microcephaly, mental retardation, hemiparesis or quadriparesis, reduced muscle tone, and hydrocephalus. Most patients with schizencephaly experience seizures.
Individuals with schizencephaly are generally treated with physical therapy, prescribed anti- convulsants to control seizures, and placement of a shunt for hydrocephalus.
What is cerebrospinal fluid?
Cerebrospinal fluid (CSF) is a clear, colorless fluid that surrounds the brain and spinal cord, protecting them from injury. CSF is mostly made up of water with a few trace proteins, electrolytes, and nutrients that are needed for the nourishment and normal function of your brain. CSF also serves the brain by carrying away waste products from surrounding tissue.
Cerebrospinal fluid production and absorption
Under normal conditions, the brain produces an amount of CSF equal to what is absorbed by the body each day. Approximately 80 to 90 percent of CSF is produced by the choroid plexus. The choroid plexus–found in the lateral, third and fourth, ventricles–is a network of blood vessels covered by a tissue membrane that secretes newly formed CSF. The average person, including older infants, produces approximately 20 milliliters (ml) of CSF per hour (about 500 ml, or a pint, per day).
The average volume of intracranial CSF (the fluid that is within the brain at any one time) is 125 to 150 ml, of which approximately 90 to 100 ml can be found in the subarachnoid space which surrounds the brain and spinal cord.
CSF is constantly being produced, flowing through, bathing, protecting, and cleansing the structures of your brain before it is reabsorbed into the bloodstream. There is a threefold turnover of CSF within a 24-hour period.
Flow of cerebrospinal fluid
The flow of CSF follows a somewhat predictable pattern throughout the brain and spinal column. Cerebrospinal fluid is produced mainly by the choroid plexus of the lateral ventricles. CSF flows from the lateral ventricles of the brain through the foramen of Monro (a short passageway that extends down from the lateral ventricles) on its way to the third ventricle. From there, the CSF passes through the narrow passageway of the cerebral aqueduct on its way to the fourth ventricle. The cerebral aqueduct is also known as the aqueduct of Sylvius. It is here that the most common cause of hydrocephalus can be found–aqueductal stenosis.
CSF exits the fourth ventricle by way of the foramina of Luschke and Magendie, where it enters the subarachnoid spaces. The fluid continues to flow over the brain to the arachnoid granulations (or villi) in the superior sagittal sinus where it is reabsorbed. The superior sagittal sinus is a venous channel that runs between the left and right hemispheres of the brain. It extends down to the back of the head where it splits in two, creating the transverse sinuses, which then turn into the internal jugular veins that return blood to the right atrium of the heart. Arachnoid villi, located in the subarachnoid space, permit the flow of CSF from that space to the superior sagittal sinus, as well as other large channels.
The brain in a nutshell
The brain is the nerve center and is by far the most complex organ in the human body. The primary function of the brain is to control the body. It regulates breathing and circulation, and controls the functions of the body's vital organs. The brain is also responsible for analyzing and remembering everything that you see, touch, hear, taste, and smell. For instance, when you reach down to touch a flower, the nerves in your fingertips send an impulse to the parietal lobe of your brain, which identifies the sensation.
To communicate effectively with neurosurgeons, patients who have hydrocephalus need to become familiar with the basic structures of the brain. Your neurosurgeon will talk about the various structures of the brain, and by being familiar with their location and functions, you will better understand what she is talking about. Learning about some of the terms and functions of the brain will allow you to more actively participate in your care. After some experience with the condition, you will find yourself talking about ventricles, hemispheres, lobes, the cerebellum, cranial nerves, and possibly other parts of the brain you didn\306t know existed.
The brain is divided into sections that control different bodily functions. The effect that hydrocephalus has on an area of the body greatly depends on where the blockage or abnormal accumulation of CSF is located. If there is a build-up of fluid near the frontal lobes of the brain, you could experience difficulty with motor skills, since the frontal lobe houses the motor cortex. Likewise, if there is a arachnoidal cyst that is placing pressure on the occipital lobe, your vision might be affected.
Responses on one side of the brain control actions on the opposite side of the body. For example, if you want to move your right arm, a signal is sent to the motor cortex of your left frontal lobe. This signal is then sent to the muscles of your arm to perform and control the movement. If there is a cyst or tumor placing pressure on the right side of the brain, it will affect the functions of the left side of the body controlled by the area where the cyst or tumor is located.
This article gives you an overview of the structures of the brain and discusses some of their functions. It first looks at the outermost structures of the brain, the meninges, then at the middle of the brain where the ventricles are located, and finally moves inside to the core of the brain, the brain stem.
Meninges
The meningeal layer surrounds the brain and spinal cord and protects them from injury. CSF acts as a cushioning device between the meninges, gray matter, and the inside of the skull. The meninges consist of three separate layers: the dura, arachnoid, and pia mater.
The outermost meningeal layer is the dura mater. The dura mater is a tough, inelastic membrane that consists of two layers fused together. The outer layer of the dura mater is similar to the periostium, and the inner layer is called the dura.
The area between the dura and arachnoid layers is known as the subdural space. When a shunt overdrains, it reduces the volume of CSF within the ventricles, causing the brain to move inward away from the meninges. As the brain moves inward, blood vessels in the arachnoid layer of the meninges are torn, forming a subdural hematoma (a pocket of blood) between the arachnoid and dura layers. Overdraining of the ventricles and subdural hematomas are just one of many possible complications of having a shunt.
The next meningeal layer is the arachnoid. This fine, cobweb-like layer covers the brain and spinal cord, and contains many large blood vessels. Unlike the dura, the arachnoid mater has an elastic quality. The area between the arachnoid layer and the next, the pia mater, is known as the subarachnoid space. CSF flows through the subarachnoid space, over the surface of the brain and spinal cord.
The innermost meningeal layer is known as the pia mater. The pia mater hugs the surface of the brain and spinal cord, and is filled with blood vessels that supply the nerve tissue below.
The meninges extend downward between the cerebral hemispheres (the cerebrum) to create the falx cerebri, and between the occipital lobes of the cerebrum and cerebellum to form the tentorium. The falx cerebri is what divides the left and right hemispheres of the brain, while the tentorium is what separates the upper and lower sections of the brain.
Cerebral hemispheres
The brain is divided into two cerebral hemispheres, which are commonly referred to as the left and right hemispheres. When combined, the cerebral hemispheres make up the cerebrum, which is the largest and most highly developed part of the brain.
The left and right hemispheres are separated by the longitudinal fissure, where the falx cerebri of the dura is located. The left and right cerebral hemispheres are joined together at the center of the brain by the corpus callosum. The corpus callosum is a broad band of fibers which allows one side of the brain to communicate with the other. The cerebral hemispheres are each made up of four pairs of lobes: frontal, temporal, parietal and occipital.
The frontal lobes are located at the front part of each cerebral hemisphere and extend back to about the middle of the brain. The frontal lobes make up approximately one-third of each hemisphere of the brain. The lower region of the left frontal lobe, known as Broca's area, is responsible for initiating speech. The prefrontal cortex, which is located at the front of each frontal lobe, plays a role in memory, social behavior, learning, judgment and personality.
Just forward of the central sulcus, located at the posterior margin of the frontal lobe, is the motor cortex. The motor cortex is responsible for controlling voluntary movements of the muscles and limbs of the body. The central sulcus, which separates the frontal and parietal lobes, begins at the top of the hemisphere and extends downward until it reaches the lateral sulcus.
The temporal lobes are located at the side of the brain, within the temple of the cranium. They are separated from the frontal lobes by a cleft called the lateral fissure. The lateral fissure is an in- folding of the frontal lobe that runs laterally between the frontal and temporal lobes. The upper region of the temporal lobe is associated with the sense of hearing. The inner region of the temporal lobe is responsible for memory.
The parietal lobes are situated above the temporal lobes and between the frontal and occipital lobes. Located within the parietal lobe is the primary sensory area, which is responsible for receiving sensations from the body. Abnormalities in this area of the brain can be associated with reading and learning disabilities.
The occipital lobe is located in the back of the brain, behind the parietal and temporal lobes and above the cerebellum. The occipital lobe is responsible for interpreting what is seen with the eyes.
Ventricular system
The ventricular system of the brain is made up of four chambers, or ventricles, which are connected to each other by way of narrow passages, called foramen. As mentioned earlier, CSF is produced in the ventricular system by the choroid plexus. The CSF flows from the ventricles into the subarachnoid space, and over the surface of the brain and spinal column. Hydrocephalus occurs when there is an obstruction of one of the ventricles or ventricular foramina (CSF passageways) that restricts the flow of CSF either within the ventricular system, the subarachnoid space, or the cisterns (reservoirs for CSF). The ventricular foramina consist of the intraventricular foramina (or the foramen of Monro), which connect the lateral ventricles with the third ventricle, and the foramina of Luschke and Magendie (located in the fourth ventricle) which provide a means for CSF to exit the ventricular system. (Foramina is the plural of foramen.)
The third and fourth ventricles are connected to each other by the cerebral aqueduct, also known as the aqueduct of Sylvius. This is the most common place for non-communicating hydrocephalus to occur, as it is the smallest passageway in the ventricular system. The foramina of Luschke and Magendie are also found in the fourth ventricle. The foramen of Magendie protrudes from the back, and the foramina of Luschke extend from each side of the fourth ventricle. The foramina of Luschke and Magendie are passages where CSF exits the ventricular system over the cerebellum into the subarachnoid space and down to the spinal cord.
The two largest ventricles are known as the lateral ventricles. They are commonly referred to by their left-right position (i.e., left lateral ventricle or right lateral ventricle). The lateral ventricles can also be referred to as the first (left lateral) and second (right lateral) ventricles. Each lateral ventricle lies within its respective cerebral hemisphere (i.e., the left lateral ventricle lies within the left hemisphere of the brain, and the right lateral ventricle lies within the right hemisphere).
The lateral ventricles, although one structure, have three different horns which extend into different lobes of the brain. The anterior horns extend forward into the frontal lobes. The posterior horns extend backward into the occipital lobes, and the inferior horns project downward into the temporal lobes. The area between the posterior and inferior horns of the lateral ventricles is known as the atrium, or trigone, located within the parietal lobes. The structure of the lobes and how they fit together create the chambers of the ventricular system.
The lateral ventricles are connected to the third ventricle by the interventricular foramen (more commonly known as the foramen of Monro). The third ventricle is located at the center of the brain, which is also home to the hypothalamus and the thalamus. The hypothalamus regulates body temperature, thirst, emotions, sleep, hunger, water balance and sexual behavior. The thalamus is the relay station of the brain. All incoming messages to the brain, with the exception of the sense of smell, enter the thalamus before being transmitted to the primary sensory cortex in the parietal lobe.
The fourth ventricle is bordered by the medulla and the pons in the front, and the cerebellum behind, with the aqueduct of Sylvius extending upward into the third ventricle.
Cerebellum
Located below the occipital lobes and behind the brain stem, the cerebellum is made up of two distinct-looking hemispheres. The cerebellum is primarily responsible for coordinating movements and muscle tone, and controlling the body's sense of balance.
Hydrocephalus can be caused near the cerebellum when there is an increase of intracranial pressure (ICP) that forces the tonsil of the cerebellum down onto the foramen magnum. The tonsil of the cerebellum is located near the base of the cerebellum. Raised ICP forces the tonsil against the brain stem and can cause an obstruction of CSF flow from the fourth ventricle. This form of non-communicating hydrocephalus can result in severe respiratory and cardiac distress, due to its pressure on the lower region of the medulla.
Brain stem
The structure that connects the brain with the spinal cord is called the brain stem. The brain stem is made up of three sections: the pons, the medulla, and the midbrain. The pons is responsible for control of facial movement, as well as some eye movements, while the medulla controls heart rate and breathing.
For more information, you can also see this Wikipedia Article
Taken from:
What is a shunt And Why Is It Necessary?
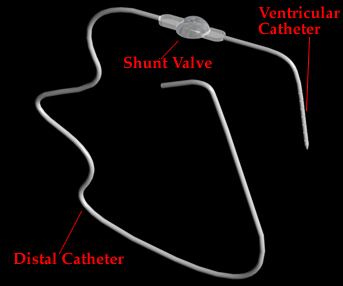
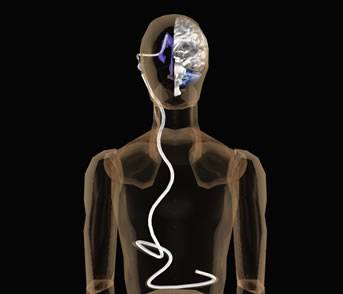
A shunt is a narrow tube which is placed in the ventricles of the brain for the purpose of draining excess spinal fluid. The shunt runs under the skin along the scalp and neck and empties into the abdominal peritoneal cavity whereby the fluid can be absorbed by the body. This type of shunt is called a VENTRICULO-PERITONEAL SHUNT. Less frequently, the end of the shunt is inserted into one of the heart's chambers and is called a VENTRICULO-ATRIAL SHUNT.
Many premature babies develop intraventricular hemorrhages. If the hemorrhage is severe enough, a blood clot forms after the bleeding. The clot causes a blockage in the normal flow of spinal fluid around and within the brain and spinal cord by obstructing the ventricles. When there is an obstruction, the fluid builds up, causing the baby's fontanel to become full and tense. This makes the head circumference grow at a faster than normal rate. Pressure continues to increase within the ventricles, and if not relieved. It may cause injury to the brain.
Other babies, often full term, may be born with hydrocephalus. The condition may be associated with another problem such as Spina Bifida or may occur alone. Irregardless of the cause, the pressure of the spinal fluid with the ventricles must be relieved to prevent damage to the brain.
HYDROCEPHALUS
The word hydrocephalus is made of two Greek words: hydro meaning fluid and cephalus meaning head. This buildup of fluid causes a buildup of pressure inside the head. If this condition is not diagnosed and treated promptly, the consequence could be a disabling affliction or even worse, it could be fatal.
The key to correction of the build-up of cerebrospinal fluid (CSF) is a relatively simple device called a shunt. A shunt is a plastic tube that is approximately the diameter of a pen filler. It varies in length depending on the patient. There are many type of shunts, but that all perform basically the same function: that is, of course, to drain off the excess CSF. After a shunt is in place, there are possibilities of complication. One possible complication is the rejection or adverse reaction to the shunt. Other problems include the disconnected shunt, the shunt being blocked, and the shunt that has become too short due to the growth of the child. There is also the possibility of infection.
SHUNT FAILURE
Diagnosis of shunt failure is probably one of the most important responsibilities of the parent or guardian of a hydrocephalic child or adult. An example of an improper diagnosis is a child who is blind because her shunt failure was not properly diagnosed. Therefore, as a parent, spouse or care giver, one should know the symptoms of shunt failure and be willing to accept the reality that their child, spouse, or the person they are caring for will need to have to shunt revised from time to time. It is extremely important to ask the neurosurgeon about the symptoms of shunt failure. Some possible symptoms are bulging fontanel (soft spot in a baby's head), change of appetite, sunsetting eyes, vomiting, lethargy, irritability, seizures, headaches and swelling or redness along the shunt tract.
Hydrocephalus may cause other types of problems Some of the most prevalent include visual problems and problems related to motor coordination and speech in these cases, therapy is required and usually very successful. There are also individuals who have no apparent side effects and lead perfectly normal lives. A good number of patients have very few revisions.
Information taken from: